About Transarterial Radioembolization (TARE)
Transarterial Radioembolization (TARE), also known as Selective Internal Radiation Therapy (SIRT), is a minimally invasive, image-guided procedure used to treat liver cancer, especially hepatocellular carcinoma (HCC) and certain metastatic liver tumors. In this procedure, a specialized interventional radiologist inserts a thin catheter through an artery (usually in the groin or wrist) and guides it to the blood vessels supplying the liver tumor. Tiny radioactive microspheres (commonly Yttrium-90) are then delivered directly into the tumor’s blood supply, where they lodge in the small vessels and release targeted radiation to destroy cancer cells while minimizing damage to surrounding healthy liver tissue. TARE is commonly recommended for patients who are not suitable for surgery or liver transplant and is especially useful in cases where blood flow blockage is risky, such as portal vein thrombosis. The procedure usually requires a short hospital stay and helps shrink tumors, slow disease progression, and improve quality of life.
Key Highlights
Transarterial Radioembolization (TARE) is a minimally invasive procedure that requires careful evaluation of liver function, tumor location, and overall health before treatment. It is an effective option for controlling liver tumors by delivering targeted internal radiation directly to the tumor through the liver’s blood vessels. While TARE is generally well tolerated, it may cause temporary side effects such as fatigue, mild abdominal discomfort, nausea, and loss of appetite. After the procedure, patients are monitored in the hospital for a short period to ensure stable recovery and to manage any symptoms. Most patients can return to normal daily activities within a few days, and follow-up imaging (CT/MRI) and blood tests are done to evaluate tumor response. In some cases, additional treatment sessions or combined therapies may be recommended based on the patient’s condition and clinical outcomes.
Who is this surgery for?
Transarterial Radioembolization (TARE), also known as Selective Internal Radiation Therapy (SIRT), is recommended for patients with liver tumors who are not suitable candidates for surgery or liver transplant. It is commonly used to control tumor growth, shrink tumors, and improve survival outcomes by delivering targeted internal radiation directly to the liver tumor through its blood supply.
Candidates Who May Benefit From TARE
1. Hepatocellular Carcinoma (HCC)
TARE is most commonly recommended for patients with primary liver cancer (HCC), especially when tumors are confined to the liver and cannot be surgically removed. It is often used for:
- Intermediate-stage liver cancer (BCLC stage B)
- Advanced-stage liver cancer with limited liver involvement
- Large liver tumors not suitable for surgery
- Patients waiting for liver transplant (bridge therapy)
2. Liver Metastases (Secondary Liver Cancer)
TARE may also be used for cancers that have spread to the liver from other organs, such as:
- Colorectal cancer liver metastases
- Neuroendocrine tumor metastases
- Breast cancer metastases (selected cases)
- Other solid tumor liver metastases (case-dependent)
3. Patients with Portal Vein Thrombosis (PVT)
TARE is often preferred over TACE in patients with portal vein thrombosis, as it does not usually cause major blockage of blood flow and can still deliver effective tumor control.
4. Patients Not Eligible for Surgery
TARE is often recommended for patients who cannot undergo surgery due to tumor size, tumor location, multiple lesions, or medical conditions such as:
- High surgical risk due to age or comorbidities
- Multiple tumors confined to the liver
- Large tumors not suitable for surgical removal
- Reduced liver reserve (selected patients)
5. Tumor Control Before Surgery or Transplant
TARE may be used as a pre-treatment approach to control tumor progression and improve eligibility for surgery or transplant, including:
- Downstaging liver tumors to meet transplant criteria
- Shrinking tumors before surgical resection
- Preventing tumor growth while waiting for transplant
6. Patients with Good Liver Function
TARE is most effective and safer in patients whose liver is still functioning well. It is typically recommended for patients with:
- Child-Pugh A or early Child-Pugh B liver function
- Stable bilirubin and liver enzyme levels
- No major symptoms of liver failure
Who Is Not Typically a Suitable Candidate?
TARE may not be recommended for individuals with:
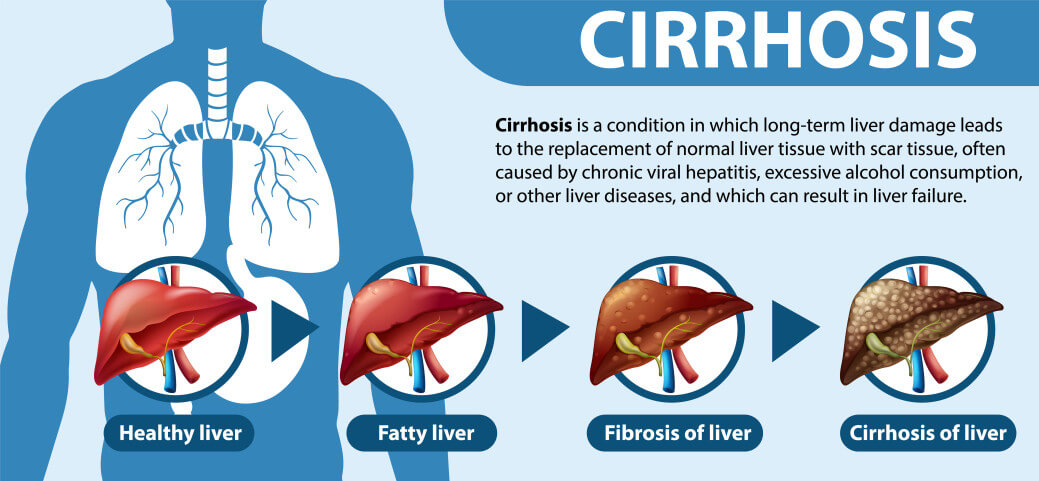
- Severe liver failure or decompensated cirrhosis
- Very high bilirubin levels or poor liver reserve
- Extensive tumor spread outside the liver
- Severe kidney dysfunction
- Uncontrolled infection or sepsis
- High lung shunting (risk of radiation exposure to lungs)
- Severe blood flow to stomach/intestine (risk of radiation injury)
How Candidates Are Evaluated
Before undergoing TARE, patients undergo a detailed evaluation to confirm eligibility and ensure radiation safety. This may include:
- Blood tests (LFT, CBC, kidney function, clotting profile)
- Imaging tests such as CT scan, MRI, or ultrasound of the liver
- Angiography mapping to evaluate liver blood vessels
- MAA scan to measure lung shunt fraction and radiation distribution
- Assessment of liver function (Child-Pugh score, MELD score)
- Evaluation of tumor size, location, and arterial blood supply
- Consultation with interventional radiology and oncology specialists
How to prepare
Preparing for Transarterial Radioembolization (TARE), also known as Selective Internal Radiation Therapy (SIRT), involves completing detailed medical evaluations, mapping the liver blood vessels, adjusting medications, and understanding what to expect before and after the procedure. Proper preparation helps reduce complications and ensures safe delivery of targeted radiation to the liver tumor.
1. Complete the Pre-TARE Evaluation
Before undergoing TARE, your doctor will perform a thorough evaluation to confirm that the procedure is safe and appropriate for your condition.
- Blood tests (Liver function test, Kidney function test, CBC, clotting profile)
- Imaging scans (CT scan, MRI, ultrasound of the liver)
- Tumor assessment and staging
- Assessment of liver function (Child-Pugh / MELD score)
- Evaluation of liver blood supply and portal vein status
- Consultation with interventional radiologist and oncologist/hepatologist
2. Liver Mapping and Planning Angiography
TARE usually requires a special planning procedure before the actual treatment. This helps doctors study blood flow and ensure radiation beads go only to the tumor.
- Diagnostic angiography to map liver arteries
- Identification of abnormal blood vessels leading to stomach or intestine
- Blocking (embolization) of risky vessels to prevent radiation injury
- Injection of a test substance (MAA scan) to evaluate radiation distribution
- Lung shunt evaluation to ensure radiation does not reach the lungs
3. Follow All Medical Instructions
Your healthcare team will provide specific instructions to prepare your body and reduce risks during the procedure.
- Take medications exactly as prescribed
- Inform your doctor about all medicines, supplements, and herbal products
- Report any fever, infection, or new symptoms before the procedure
- Follow fasting instructions (usually no food or drink for 6–8 hours before TARE)
- Get clearance if you have diabetes, heart disease, or kidney problems
4. Adjust Blood Thinners and Other Medications
Some medications may increase bleeding risk during catheter-based procedures. Your doctor may advise stopping or adjusting certain medicines before TARE.
- Blood thinners (Aspirin, Warfarin, Clopidogrel, etc.) may need temporary stopping
- Diabetes medicines may require dose adjustment on procedure day
- Inform the doctor if you are allergic to contrast dye or iodine
- Stomach-protective medicines may be prescribed to reduce radiation-related irritation
- Antibiotics may be prescribed in selected cases to prevent infection
5. Make Lifestyle and Diet Preparations
Healthy habits help improve liver stability and reduce complications during and after TARE.
- Avoid alcohol completely
- Stop smoking or tobacco use if possible
- Follow a liver-friendly diet (low salt, balanced nutrition)
- Stay hydrated as advised by your doctor
- Get enough rest before the procedure
6. Arrange Support for Hospital Stay and Recovery
TARE usually requires short hospital observation. Having support helps with safe recovery and follow-up.
- Arrange a family member or caregiver to accompany you
- Plan transportation (you may not be able to drive after the procedure)
- Prepare for 1–2 days of rest after treatment
- Keep all medical records, scan reports, and prescriptions ready
- Plan follow-up visits for blood tests and imaging scans
7. Understand What to Expect After TARE
Most patients experience mild side effects after TARE. Knowing them in advance helps reduce anxiety and ensures timely medical care.
- Fatigue and weakness for several days
- Mild fever, nausea, or reduced appetite
- Abdominal discomfort or heaviness
- Hospital monitoring for a few hours to 1 day
- Follow-up CT/MRI scan after a few weeks to assess tumor response
- In some cases, additional treatment sessions may be required depending on tumor response
Risks & possible complications
Transarterial Radioembolization (TARE), also known as Selective Internal Radiation Therapy (SIRT), is an advanced and minimally invasive treatment for liver tumors. While it is generally considered safe and effective, it can still carry certain risks and potential complications. Understanding these risks helps patients and families prepare and know what symptoms to monitor during recovery.
Procedure-Related Risks
- Bleeding or bruising at the catheter insertion site (groin or wrist)
- Damage to the blood vessel during catheter placement
- Allergic reaction to contrast dye used in imaging
- Injury to surrounding organs due to catheter manipulation (rare)
Post-Radioembolization Symptoms
Most patients experience mild side effects after TARE, usually lasting a few days to a couple of weeks.
- Fatigue and weakness (most common)
- Mild fever
- Nausea or reduced appetite
- Abdominal discomfort or heaviness
- Temporary flu-like symptoms
Liver-Related Complications
Although TARE targets tumors precisely, radiation can still affect healthy liver tissue in some cases.
- Temporary liver function worsening (rise in bilirubin or liver enzymes)
- Radiation-induced liver inflammation (rare)
- Radiation-induced liver disease (RILD) (rare but serious)
- Ascites (fluid buildup in the abdomen in advanced liver disease patients)
Radiation-Related Complications
Since TARE uses radioactive microspheres, improper distribution may rarely cause radiation exposure to other organs.
- Radiation gastritis (stomach irritation)
- Radiation ulcers in stomach or intestine (rare)
- Pancreatitis due to accidental radiation exposure (rare)
Lung-Related Complications
In rare cases, radioactive particles may travel to the lungs, especially if lung shunting is high.
- Radiation pneumonitis (rare but serious)
- Breathing difficulty or persistent cough (rare)
Infection Risks
Although TARE is minimally invasive, infection may occur in rare cases.
- Infection at the catheter insertion site
- Liver abscess (rare, more common in patients with bile duct procedures)
- Fever due to infection (needs medical evaluation)
Gallbladder and Bile Duct Complications
In some cases, radioactive microspheres may affect the gallbladder or bile ducts.
- Gallbladder inflammation (radiation cholecystitis)
- Bile duct narrowing or injury (rare)
- Bile duct inflammation due to radiation exposure
Kidney and Contrast-Related Complications
- Temporary kidney function worsening (especially in elderly or diabetic patients)
- Contrast-induced nephropathy (rare)
- Dehydration-related kidney stress
Other Potential Complications
- Blood clot formation in l
Recovery & hospital stay
Recovery after Transarterial Radioembolization (TARE), also known as Selective Internal Radiation Therapy (SIRT), happens in stages, starting immediately after the procedure in the hospital and continuing at home over the next few days to weeks. The recovery phase focuses on managing side effects, monitoring liver function, and assessing how well the tumor responds to radiation treatment.
Hospital Stay After the Procedure
- Observation and monitoring (6–24 hours or more): Patients are closely monitored for blood pressure, heart rate, pain, and any signs of bleeding or complications.
- Catheter site care: The catheter insertion site (groin or wrist) is checked regularly to prevent bleeding, swelling, or infection.
- Short hospital stay: Many patients are discharged the same day or within 1 day, while some may stay 1–2 days depending on liver condition and symptoms.
- Hydration and medication support: IV fluids and supportive medications may be given to reduce nausea, protect the stomach, and support recovery.
- Early mobility: Patients are encouraged to start light movement after a few hours to support circulation and reduce clot risk.
Pain and Symptom Management
Most patients experience mild discomfort rather than severe pain after TARE. Fatigue is the most common symptom. The medical team may provide medications for pain relief, nausea control, and stomach protection to ensure comfort during recovery.
Monitoring During Hospital Stay
- Regular blood tests to check liver function and kidney function
- Monitoring for fever, nausea, fatigue, or abdominal discomfort
- Checking the catheter site for bleeding or infection
- Observation for rare radiation-related side effects
Recovery at Home
Most patients recover within 7–14 days, although fatigue may last longer for some individuals. Following medical advice at home is important for safe healing and better treatment outcomes.
- Rest and hydration: Adequate rest and fluids help reduce fatigue and support liver recovery.
- Medication adherence: Take prescribed medicines such as pain relievers, anti-nausea medication, and stomach-protective drugs as advised.
- Activity: Light walking is encouraged; avoid heavy lifting or strenuous activity for at least 5–7 days.
- Diet: Eat light meals initially and follow a liver-friendly diet (low-fat, low-salt) if advised.
- Follow-up scans: CT or MRI scans are usually scheduled after 6–12 weeks to evaluate tumor response.
- Long-term monitoring: Blood tests and follow-ups are required to assess liver function and treatment effectiveness.
When to Seek Medical Help
- High fever (above 101°F / 38.3°C) or chills
- Severe or worsening abdominal pain
- Persistent vomiting or inability to eat or drink
- Bleeding, swelling, or redness at the catheter insertion site
- Yellowing of the skin or eyes (jaundice)
- Breathing difficulty, persistent cough, or chest pain
- Black stools, severe stomach pain, or signs of gastric ulcer (rare but serious)
- Severe weakness, confusion, or sudden swelling in the abdomen
Your healthcare team will provide detailed recovery instructions and monitor your progress closely through follow-up blood tests and imaging to ensure safe recovery and effective tumor control.
-
Typical hospital stay: 4-5 days
-
Expected recovery time: 2-3 weeks for initial recovery; 4-6 weeks for full return to normal activities
Frequently Asked Questions
If you are considering transarterial radioembolization (tare) in India, these questions and answers can help you make a confident, informed decision.
Popular choices for transarterial radioembolization (tare) in India include Gem Hospital Perungudi, Miot Hospital Chennai, Gem Hospital Coimbatore, Nanavati Max Hospital, Kamineni Hospital, Tadigadapa, known for experienced specialists and advanced surgical infrastructure.
Look at the doctor’s years of experience, hospital association, patient reviews, and how often they perform transarterial radioembolization (tare). MediFyr helps you compare liver transplant specialists and book consultations online.
The overall cost depends on hospital category, surgeon’s experience, room type, implant or device used (if any), length of stay, tests, and post-operative care. Our team can help you get cost estimates from multiple hospitals before you decide.
Procedure cost in other countries
Here is an overview of how the estimated cost, hospital stay, and recovery time for transarterial radioembolization (tare) compare across other countries where we have data.
| Country | Estimated cost range | Typical stay | Recovery time | View details |
|---|---|---|---|---|
| India | USD 7,725 – USD 22,070 | 4-5 days | ~ 2-3 weeks for initial recovery; 4-6 weeks for full return to normal activities | Know More |
| Turkey | USD 6,003 – USD 11,005 | 4-5 days | ~ 2-3 weeks for initial recovery; 4-6 weeks for full return to normal activities | Know More |
Top hospitals for Transarterial Radioembolization (TARE) in India
These partner hospitals in India have dedicated liver transplantation teams and experience managing patients undergoing transarterial radioembolization (tare).
Had my gallbladder out at MGM....
Had my gallbladder out at MGM. The surgery itself went fine, but the first two days after were rough. Dr. Subramanian was really clear about what to expect pain-wise and adjusted my meds a couple times until we found what worked. He didn't just send me home and forget—the nurses checked in on his instructions. It wasn't fun, but I felt managed, not just processed.
Liver Transplant Specialists for Transarterial Radioembolization (TARE)
Explore experienced liver transplant specialists who regularly perform transarterial radioembolization (tare) and provide pre- and post-operative care in India.

- Years Experience
- Liver Transplant Specialist
Star Hospital Nanakramguda

- Years Experience
- Liver Transplant Specialist
Star Hospital Nanakramguda

- 9 Years Experience
- Liver Transplant Specialist
Star Hospital Nanakramguda

- 28 Years Experience
- Liver Transplant Specialist
Star Hospital Nanakramguda

- 8 Years Experience
- Liver Transplant Specialist
Lilavati Hospital

- 21 Years Experience
- Liver Transplant Specialist
Lilavati Hospital

- 12 Years Experience
- Liver Transplant Specialist
Lilavati Hospital

- 22 Years Experience
- Liver Transplant Specialist
Medanta Hospital Gurgaon

- 14 Years Experience
- Liver Transplant Specialist
Medanta Hospital Gurgaon

- 13 Years Experience
- Liver Transplant Specialist
Medanta Hospital Gurgaon

- 16 Years Experience
- Liver Transplant Specialist
Manipal Hospital Dwarka

- 31 Years Experience
- Liver Transplant Specialist
Manipal Hospital Millers Road

- 21 Years Experience
- Liver Transplant Specialist
Manipal Hospital Millers Road

- 37 Years Experience
- Liver Transplant Specialist
Gleneagles Global Hospital Chennai

- 26 Years Experience
- Liver Transplant Specialist
Gleneagles Global Hospital Chennai

- 23 Years Experience
- Liver Transplant Specialist
Gleneagles Global Hospital Chennai

- 9 Years Experience
- Liver Transplant Specialist
Apollo BGS Hospitals Mysore

- 19 Years Experience
- Liver Transplant Specialist
Apollo Hospitals Greams Road

- 16 Years Experience
- Liver Transplant Specialist
Nanavati Hospital Mumbai

- 16 Years Experience
- Liver Transplant Specialist
Nanavati Hospital Mumbai












